813.876.3636
813.876.3636
Radioiodine therapy is a treatment prescribed for an overactive thyroid gland or thyroid cancer. It involves using radioactive iodine (radioiodine) to target and destroy thyroid cells. This therapy is often recommended by endocrinologists as part of a comprehensive treatment plan.
The thyroid gland produces hormones that regulate the body’s metabolism. To do this, it requires large amounts of iodine, which is found in foods like seafood, table salt, and bread. Each molecule of thyroid hormone contains three (T3) or four (T4) molecules of iodine. Overactive thyroid glands, which are highly iodine-hungry, can be treated with radioactive iodine to destroy the excess tissue. Radioiodine has been used for over 60 years with few side effects, although high doses can cause issues like decreased taste sensation and salivary gland irritation. There is no significant increase in birth defects or second cancers from this treatment.
Before modern treatments, severe hyperthyroidism had a high mortality rate. Today, treatments include antithyroid drugs, surgery, and radioiodine. Radioiodine is the treatment of choice for hyperthyroidism caused by overproduction of thyroid hormones. The treatment involves taking radioactive iodine orally, usually in capsule form, which is absorbed by the thyroid and gradually destroys the overactive cells. It can take one to three months for the full effect. Most patients develop hypothyroidism (underactive thyroid) after treatment, which is managed with lifelong thyroid hormone replacement therapy. Occasionally, a second dose of radioiodine is needed if the initial treatment is insufficient.

The two most common types of thyroid cancer, papillary and follicular, can typically be treated with radioiodine due to their ability to absorb iodine.
If radioiodine is inadvertently administered to a woman who is subsequently discovered to be pregnant, the advisability of terminating the pregnancy should be discussed with the patient’s obstetrician and endocrinologist. This is because radioiodine can cross the placenta and potentially harm the developing fetus. Therefore, prior to administering diagnostic or therapeutic radioiodine treatment, pregnancy testing is mandatory whenever pregnancy is possible.
Small amounts of radioactive iodine are excreted in breast milk. Since radioiodine could permanently damage the infant’s thyroid, breastfeeding is not allowed during and after treatment with radioiodine. Mothers should discontinue breastfeeding well before receiving radioiodine therapy to ensure no residual radioactive iodine is passed to the infant.


Males are advised to avoid fathering a child for several months after receiving radioiodine treatment. This precaution is to allow any potentially damaged sperm to be replaced by new, healthy sperm.
Females are advised to postpone pregnancy for six months or more following radioiodine treatment. This delay helps stabilize their thyroid status for conception and reduces the theoretical risk to a developing fetus from any residual radioactivity.
Even though the amount of radioactivity retained may be small and there is no medical proof of an actual risk from radioiodine treatment, these precautions effectively eliminate direct fetal exposure to radioactivity and markedly reduce the possibility of conception with sperm that might theoretically have been damaged by exposure to radioiodine. Patients are advised to contact their physician for guidance about methods of contraception.
Regulations regarding the use of radioiodine therapy are made by the U.S. Nuclear Regulatory Commission (NRC). Physicians and hospitals that administer this therapy must have a license to administer radioiodine and must adhere to stringent regulations regarding its use.
If you have any questions before or after receiving your treatment, do not hesitate to contact your physician or your hospital radiation safety officer for clarification.
Treatment for hyperthyroidism with radioiodine is typically done on an outpatient basis, as the dose required is relatively small. Hospitalization is generally not necessary.
For thyroid cancer, the doses of radioiodine administered are significantly larger, and hospitalization may be required for several days. The duration of the hospital stay depends on:
If hospitalization is necessary, the hospital room will be prepared with protective coverings on frequently handled items (e.g., television remote, table, phone, faucet handles) and partial floor coverage to prevent contamination.
Patients should bring minimal belongings and use hospital-provided items like gowns. Disposable items (magazines, newspapers) are preferable, while important or durable items should be left at home. All personal items will be monitored for contamination upon discharge.
For several days after treatment, patients should follow these guidelines to reduce exposure to others:
Brief periods of close contact, such as handshaking and hugging, are permitted.
Depending on the amount of radioactivity administered, continued precautions may be necessary for several weeks. Your endocrinologist or radiation safety officer will provide specific recommendations.
Patients receiving radioactive iodine should carry information about their treatment to inform authorities responsible for screening for radioactive materials in public areas such as airports and subways.
If you have any further questions or concerns, contact your endocrinologist or the hospital radiation safety officer for guidance.


The amount of radioactive exposure to others during your daily activities depends on the duration of contact and the distance between you and them. For instance, someone two feet away receives only one-fourth the exposure of someone one foot away. Thus, the general principle is to avoid prolonged, close contact with other people for several days after treatment.
By following these precautions, you can minimize the risk of radioactive exposure to others. If you have any further questions or concerns, contact your endocrinologist or the hospital radiation safety officer for guidance.
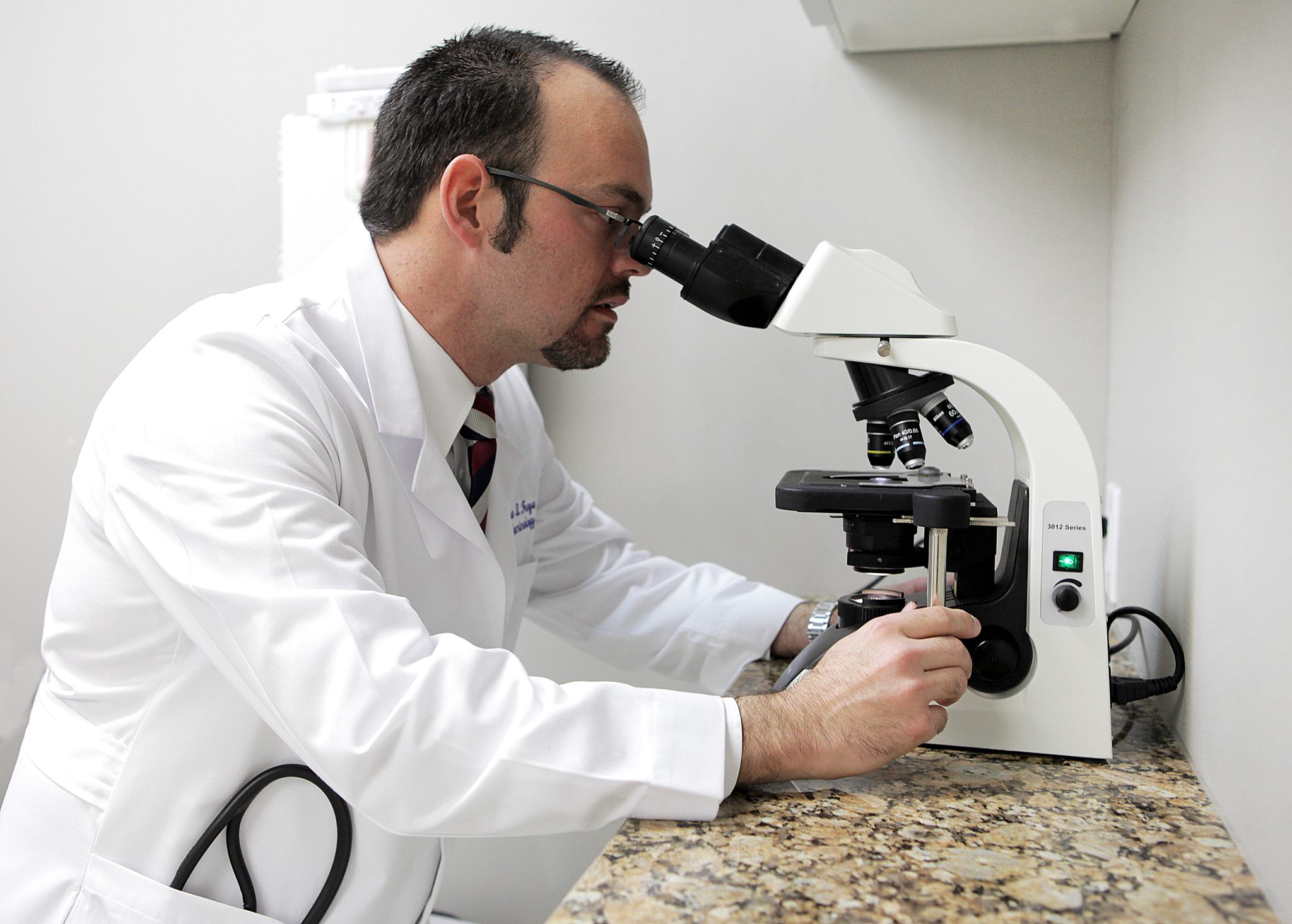
Our Endocrinologists, Dr. Carlo A. Fumero, Sean Amirzadeh, DO, Alberto Garcia Mendez, Lauren Sosdorf, and Pedro Troya, are board certified by the American Board of Internal Medicine and have a wealth of experience treating thyroid conditions. They will work with you to create a personalized treatment plan that meets your unique needs.




Tampa Office:
Zephyrhills Office:
Plant City Office: