813.876.3636
813.876.3636
Hypercalcemia is an elevated calcium (Ca2+) level in the blood, with normal levels ranging from 8.5 to 10.0 mg/dL. It can result from excessive skeletal calcium release, increased intestinal calcium absorption, or decreased renal calcium excretion. Often, it is an asymptomatic laboratory finding, but it may indicate other diseases, warranting further investigation if it persists.
1. Abnormal Parathyroid Gland Function
2. Malignancy
3. Vitamin-D Metabolic Disorders
4. Disorders Related to High Bone-Turnover Rates
5. Renal Failure
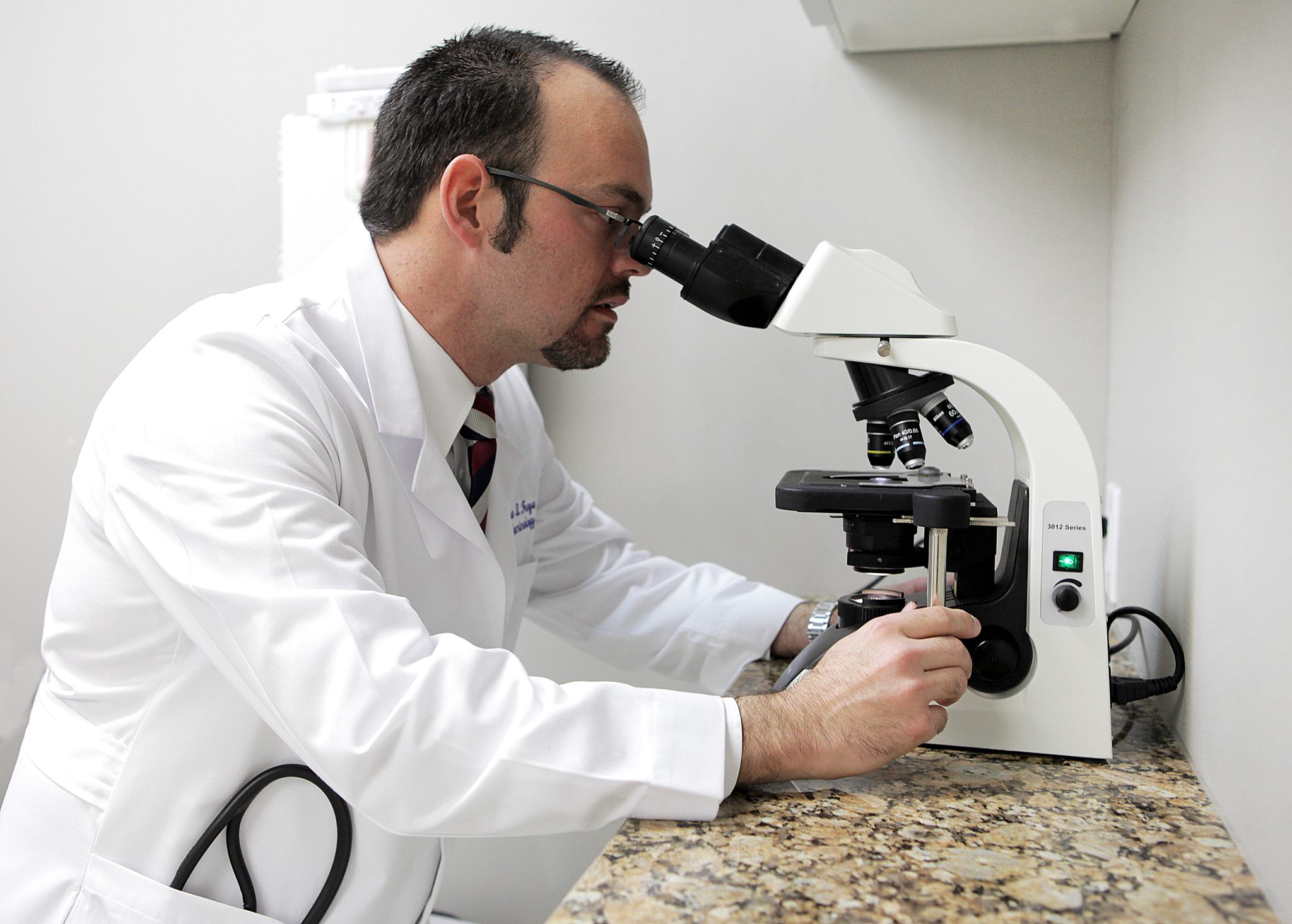

1. Addressing the Underlying Cause The key to treatment is addressing the underlying cause of hypercalcemia.
2. Initial Therapy: Fluids and Diuretics
3. Additional Therapy: Bisphosphonates and Calcitonin
4. Other Therapies (Rarely Used)
By targeting the root cause and using a combination of hydration, diuretics, bisphosphonates, and calcitonin, hypercalcemia can be effectively managed, especially in severe cases.
Our Endocrinologists, Dr. Carlo A. Fumero, Sean Amirzadeh, DO, Alberto Garcia Mendez, Lauren Sosdorf, and Pedro Troya, are board certified by the American Board of Internal Medicine and have a wealth of experience treating thyroid conditions. They will work with you to create a personalized treatment plan that meets your unique needs.




Tampa Office:
Zephyrhills Office:
Plant City Office: