813.876.3636
813.876.3636
Most people have four pea-sized parathyroid glands located behind the thyroid gland in the neck. Despite their similar names, the thyroid and parathyroid glands serve different functions. The parathyroid glands produce parathyroid hormone (PTH), which helps maintain the balance of calcium and phosphorous in the body. Hyperparathyroidism occurs when these glands secrete excess PTH, disrupting this balance.
1. Primary Hyperparathyroidism (PHPT):
2. Secondary Hyperparathyroidism:
PHPT is characterized by the autonomous production of excess PTH by the parathyroid glands, leading to elevated calcium levels (hypercalcemia).
Most people with PHPT are asymptomatic, but symptoms can include:
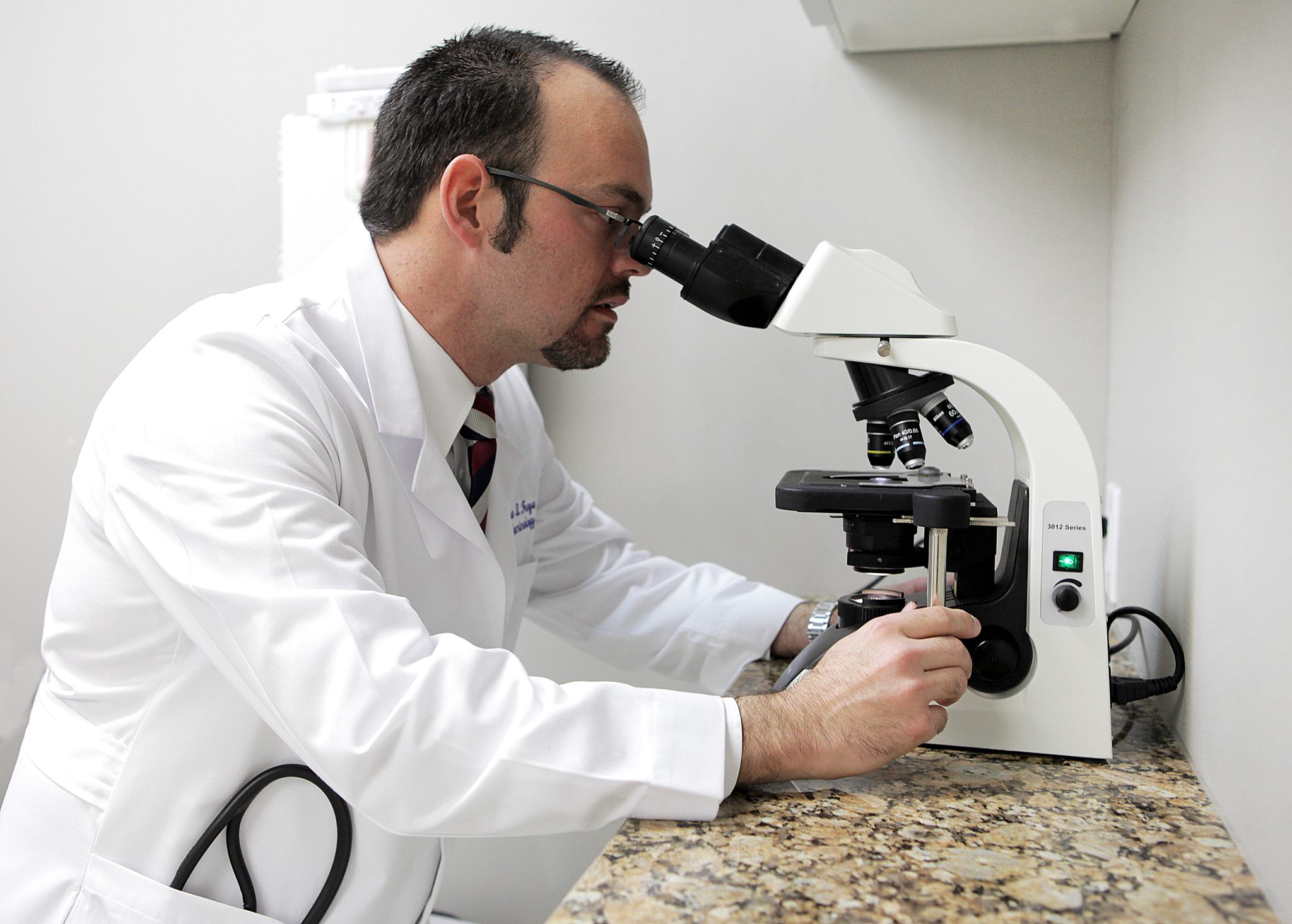

Diagnosis is based on laboratory tests showing elevated calcium and PTH levels. Confirmatory tests are essential, as calcium levels may fluctuate.
1. Surgery:
Indications for Surgery:
Types of Surgery:
Surgery has a high success rate when performed by experienced endocrine surgeons. It can lead to improved bone density, fewer fractures, and reduced kidney stones.
2. Monitoring:
3. Medications:
4. Diet and Nutrition:
By addressing the underlying cause, using appropriate surgical interventions, and monitoring, hyperparathyroidism can be effectively managed.
Our Endocrinologists, Dr. Carlo A. Fumero, Sean Amirzadeh, DO, Alberto Garcia Mendez, Lauren Sosdorf, and Pedro Troya, are board certified by the American Board of Internal Medicine and have a wealth of experience treating thyroid conditions. They will work with you to create a personalized treatment plan that meets your unique needs.




Tampa Office:
Zephyrhills Office:
Plant City Office: